While PCOS, polycystic ovary syndrome, and diabetes may seem to be unrelated at first glance—there’s actually more overlap between the two conditions than you might think.
According to the CDC, over 50% of women with PCOS eventually develop type 2 diabetes by age 40. Let’s explore why and what you can do to cope.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects approximately 1/10 American women. To receive a PCOS diagnosis, your doctor will look for two out of three of the following:
- Irregular or infrequent periods
- An overproduction of androgens, which can show up as symptoms like acne and excess body hair
- Ovarian cysts
Learn more about the most common PCOS symptoms here.
What is Diabetes?
Diabetes is a metabolic disorder that occurs when the body either doesn’t produce enough insulin (Type 1 diabetes) or becomes resistant to the effects of insulin (Type 2 diabetes). Diabetes affects the body’s ability to regulate blood sugar levels and can lead to various complications if not managed properly.
Unraveling the Link between PCOS and Diabetes
The shared underlying metabolic issue linking PCOS and diabetes is insulin resistance—which means that cells cannot properly use blood sugar for energy with the consumption of carbohydrates. With insulin resistance, blood sugar can become dangerously high, leading to health problems like excess weight and diabetes.
Excess weight can exacerbate insulin resistance, but insulin resistance also makes it difficult to lose weight, creating a vicious cycle. Since PCOS is often associated with insulin resistance, it’s important for women who are diagnosed to keep an eye on their metabolic markers to prevent diabetes.
It’s unclear what causes PCOS or insulin resistance, but family history plays a large part. In any case, losing excess weight is shown to help improve PCOS and diabetes symptoms and prevent further disease.
Preventing Diabetes When You Have PCOS
Understand Your Biomarkers
Knowledge is power! Given the increased risk, it is crucial for women with PCOS to be vigilant about monitoring their health. Check your insulin, fasting glucose, A1C, and cholesterol regularly! Our Weight Biology Kit is designed to make it affordable and easy to monitor these metabolic markers from home (and explain what they mean) so you understand exactly what’s going on with your health.
Pre-diabetes doesn’t normally have symptoms, which is why getting blood work done is important. But some warning signs of diabetes include:
- Increased thirst
- Frequent urination
- Increased hunger
- Fatigue
- Blurred vision
- Numbness or tingling in the feet or hands
- Frequent infections
- Slow-healing sores
Ideally, you can catch any metabolic red flags before reaching a pre-diabetes diagnosis. But the good news is that it is possible to reverse pre-diabetes if you catch it in time.
Make Lifestyle Adjustments
We’ve all heard about how important losing weight is for health outcomes, but that doesn’t make it easy to do! That’s why it’s so helpful to have a clear understanding of your personal biology when making a plan for managing your symptoms.
Once you know exactly what metabolic issues are impacting you, you can treat them with the appropriate medical care and lifestyle changes like diet, exercise, and supplements.
Sticking to a diet with PCOS can be hard because of an imbalance in blood sugar levels, causing cravings and fatigue. For this reason, many women benefit from medication like Metformin or Ozempic to help stabilize blood sugar and make losing weight easier.
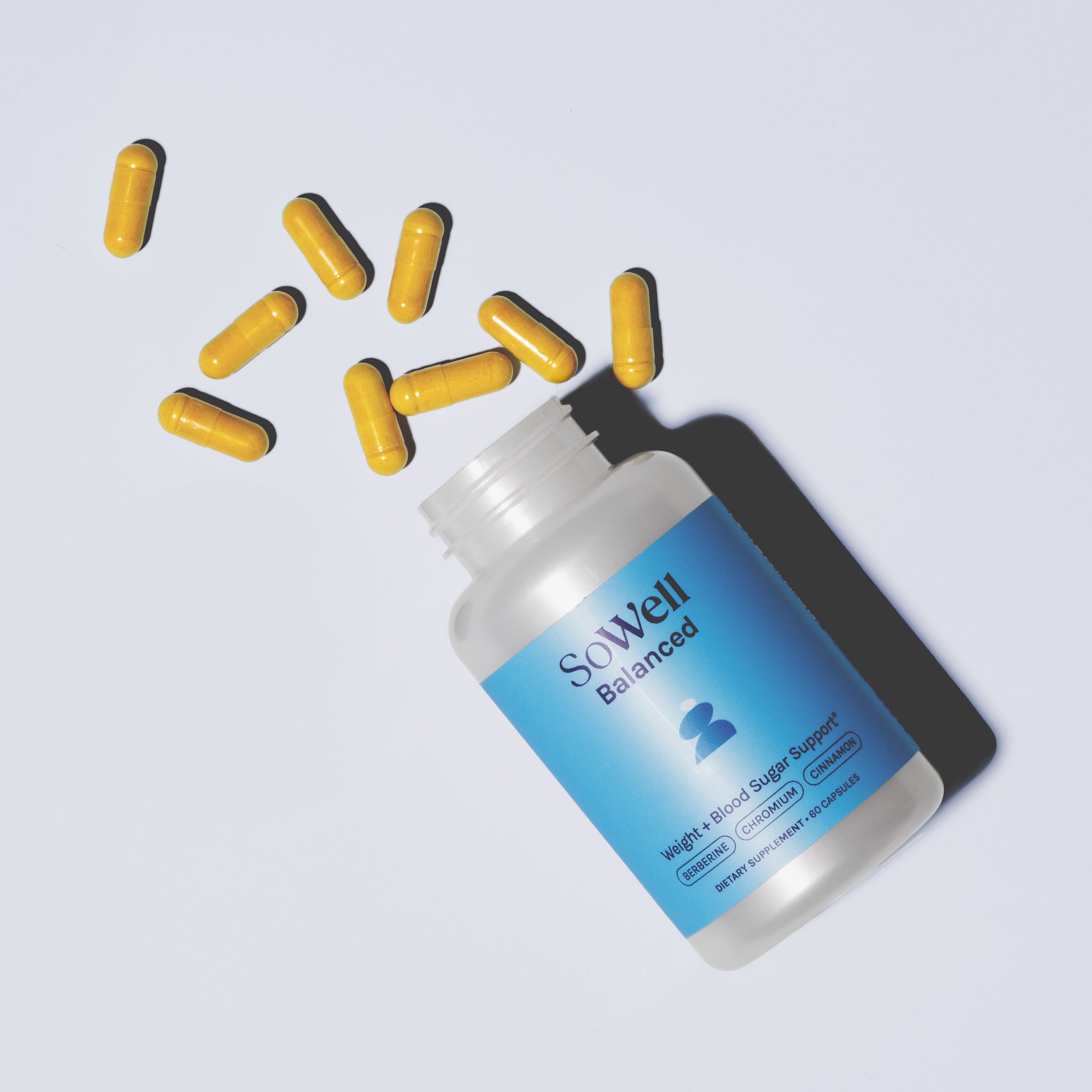
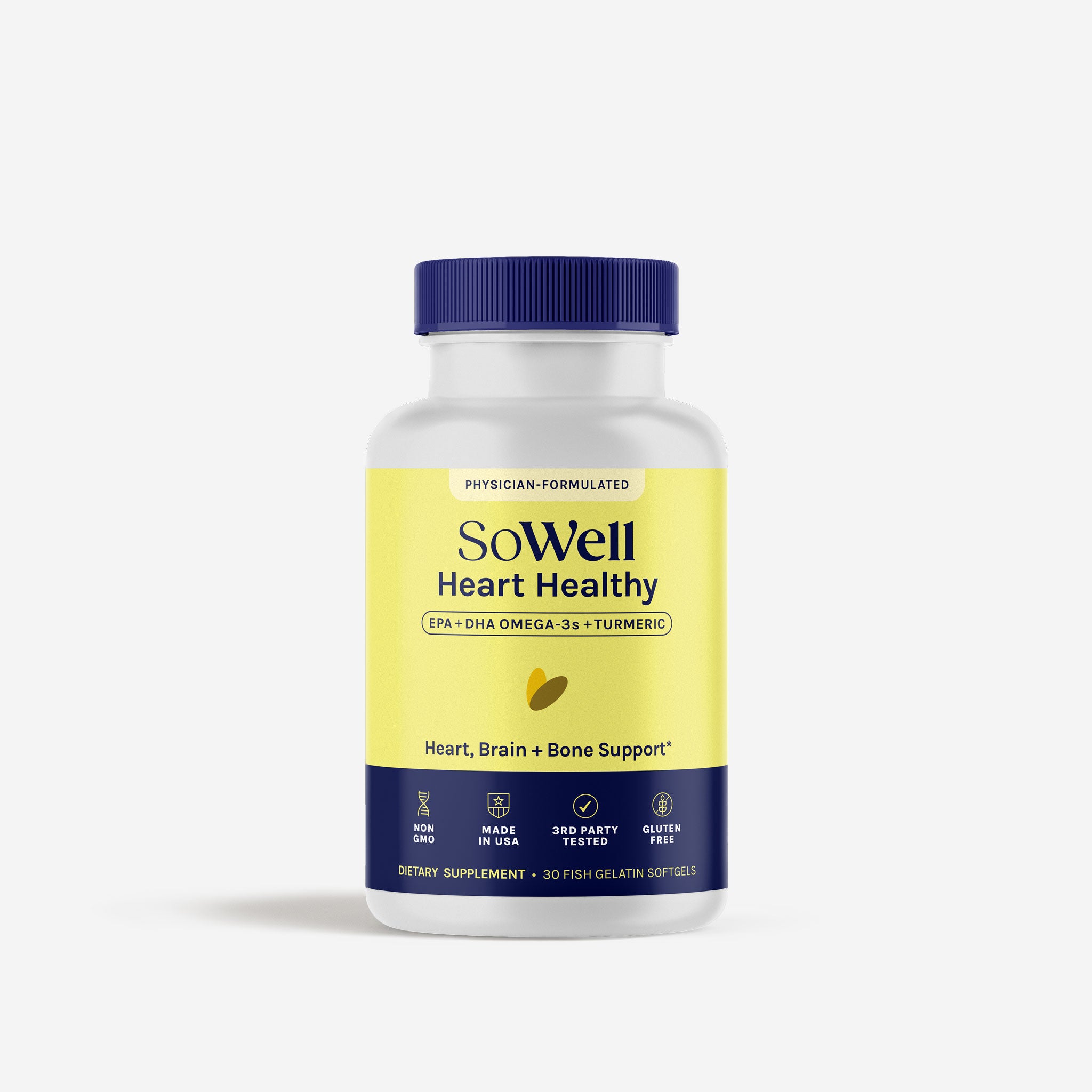
With the right medical help, following a PCOS-friendly diet—and accompanying weight loss—gets a lot easier! Even the right supplements can help to support blood sugar levels and metabolic function, adding extra support to the journey.
To see if you qualify for SoWell’s tele-health metabolism and weight care program, click here.
Living with PCOS and Diabetes
Since insulin resistance is foundational to both PCOS and diabetes, treating both involves managing blood sugar and improving insulin sensitivity. Medications like Metformin and Ozempic are helpful for both conditions and can also help support weight loss.
Significant weight loss has also been linked to seeing remission in Type 2 diabetes and sometimes helps to make symptoms of PCOS less severe. The most successful diet is the one that works for you—but the top three that have the best evidence for them in relation to these conditions are a low-carb diet, the Mediterranean diet, and a low-glycemic diet.
And even without weight loss, there’s evidence that exercise can improve insulin sensitivity. Resistance training is the best bet if you’re going to start an exercise program since building muscle can help boost the metabolism at rest.
In addition to following the proper medication schedule and diet and exercise program, supplements can help to naturally improve blood sugar and symptoms related to PCOS. Someone suffering from both PCOS and diabetes would benefit from supplementing with a blend like GetSoSynced, which features Myo-inositol, D-Chiro inositol, B vitamins, and magnesium to help regulate menstrual cycles and balance blood sugar.
Most importantly, be proactive. No matter where you are on your health journey, making positive changes now can help prevent complications and lead to a happier, healthier life overall.