Polycystic ovary syndrome (PCOS), also known as polycystic ovarian syndrome, is the most common hormonal disorder affecting women of child-bearing age. Its effects on hormone levels can cause infertility, skin issues, abnormal hair growth, and weight gain.
Medical advice is often pretty simple: Lose weight to improve your PCOS symptoms.
Not very empathetic, right?
Many women with PCOS feel it’s impossible to lose weight, but they know it’s important to manage or heal their condition. In fact, most of my patients feel so discouraged when we first meet that they’ve all but given up on getting to a healthier weight. (But that’s why I’m here to help!)
Is it possible to lose weight with PCOS? It is possible to lose weight with PCOS using evidence-based methods like targeted dietary changes, appropriate exercise, supplements, and more.
It may take longer than for someone without a hormonal imbalance, but persistence and long-term lifestyle changes pay off.
I developed The Weight Biology Kit to help people, including women with PCOS, identify what’s keeping them from losing weight. It’s super easy to use, and you’ll receive lab results in just 2-5 days!
Why is weight loss so hard with PCOS?
Weight loss is difficult when you have PCOS primarily due to insulin resistance.
Women with PCOS have higher levels of male hormones called androgens. High androgen levels contribute to many of the most obvious symptoms of PCOS, like an increase in unwanted body hair, irregular periods and menstrual cycles, and insulin resistance.
Insulin helps your body process glucose (sugar) for energy. Barriers to healthy insulin sensitivity can raise your blood sugar levels, mess with your appetite and triggers that help you feel full, and lead to weight gain.
PCOS can also increase cortisol levels, a potential cause of resistant belly fat.
Many women struggling with PCOS weight gain find themselves in a cycle of yo-yo dieting and unhealthy patterns of binge eating or overeating. It’s a double-edged sword. It’s harder to lose weight with PCOS, but losing weight significantly improves symptoms in the long term.
The health risks of being overweight with PCOS include:
- High cholesterol
- High blood pressure
- Obstructive sleep apnea
- A higher risk of heart disease
- Type 2 diabetes
Obesity worsens symptoms of PCOS, but losing weight can dramatically improve what you’re experiencing with PCOS, including its effects on insulin sensitivity.
Lifestyle changes are typically the first course of action for women struggling with PCOS and body weight. The right combo for a healthy BMI with PCOS may require some trial and error (and support!), but you can get to a healthy weight and keep it off once you find what works for you.
1. Adjust your diet.
A healthy lifestyle begins with a healthy diet. A nutrition specialist or dietitian can help you make personalized changes to your diet, especially if you’re having trouble getting started or dealing with other conditions like metabolic syndrome.
Generally, a diet like the Mediterranean diet rich in healthy fats, whole grains, and plenty of fresh fruits and veggies is best for most people (with or without PCOS). Going Mediterranean offers the added bonus of reducing chronic inflammation, another potential barrier to long-term weight loss.
Let’s take a closer look at gradual changes you can make to your diet to combat body fat.
Increase your protein intake.
A diet higher in protein can reduce food cravings and keep you feeling full longer than a diet high in carbs or fats. Protein can also improve blood sugar levels and boost your metabolism, all good things when you’re struggling with keeping weight off.
Healthy sources of protein include almonds, Greek yogurt, eggs, lean poultry, and oatmeal. If you know you’re low on protein, try keeping a food diary to track your progress. Shoot for protein to account for about 30% of your daily diet.
Eat fewer carbs and sugar.
Insulin resistance makes it difficult for your body to process carbs and sugars (simple carbohydrates). If you’re already dealing with sugar crashes, consuming refined carbs like processed breads and pastas will only make it worse.
A high-protein, low-carb diet like keto may help symptoms of PCOS for some, especially if you like set guidelines to follow and need to get your insulin in check quickly. For others, the idea of monitoring fats and proteins may be a barrier to long-term changes.
Consuming fewer refined carbs and processed sugars in favor of high-fiber whole grains is a great start.
Consume more fiber.
If you’re dealing with PCOS belly, increasing your fiber intake can improve blood sugar levels and reduce belly bloat. A high-fiber diet is a key component of a healthy gut microbiome.
Eat a diet rich in fresh fruits and vegetables, legumes, and whole grains to boost your fiber intake.
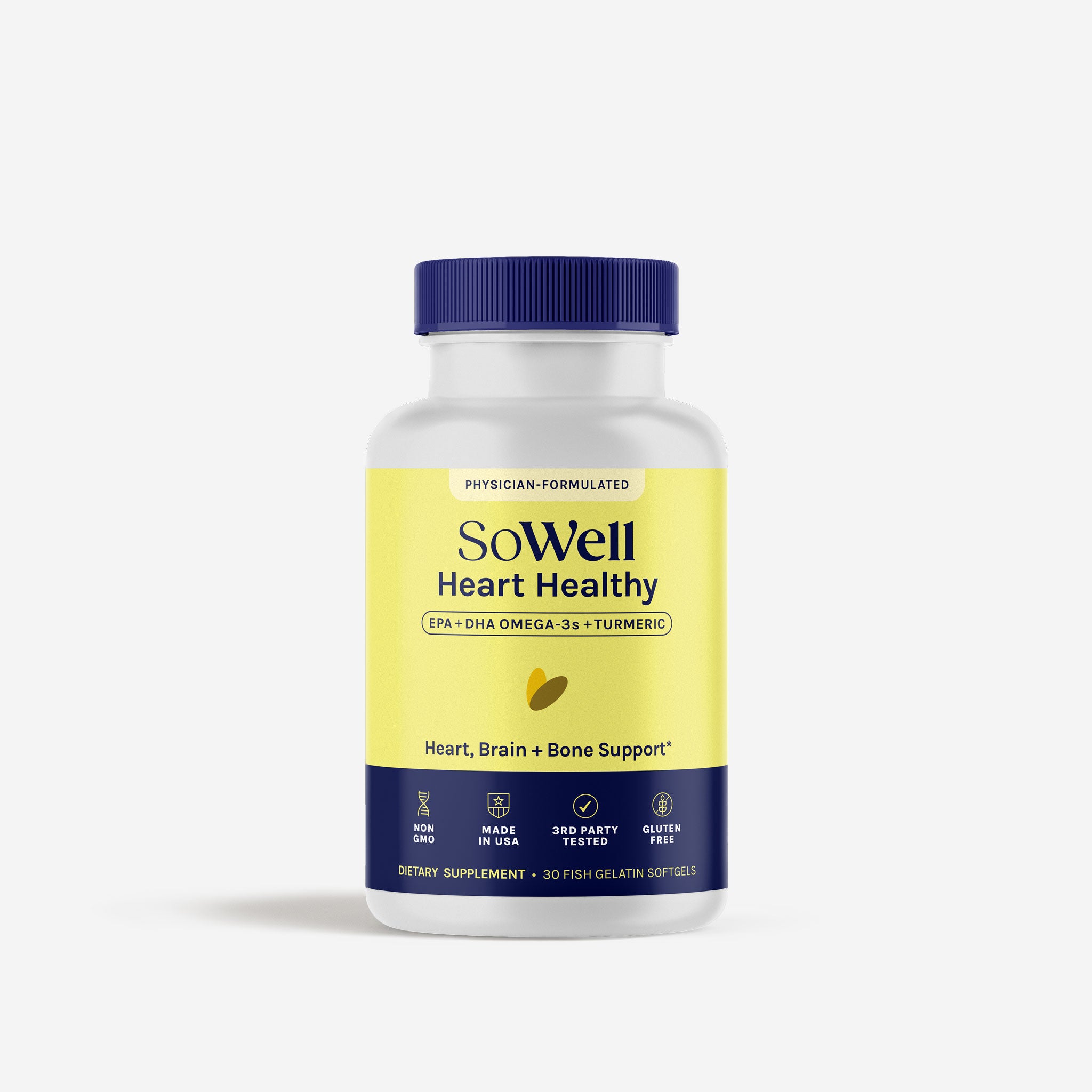
Incorporate more healthy fats into your meals.
A solid PCOS diet incorporates a variety of healthy mono- and polyunsaturated fats, also referred to as “healthy fats.”
Seeds, nuts and nut butter, avocados, and extra-virgin olive oil are all great sources of healthy fats that may already be in your pantry. Add fish like salmon and mackerel to round out a delicious dinner.
Eat fewer processed foods.
Processed foods like sugary breakfast cereals, lunch meat, and many of the ready-to-eat meals you’ll find in the freezer aisle are on the naughty list if you want to fight PCOS weight gain. As with any diet, fresh is always best.
Get to know food labels. Aim for as many whole foods as possible, and avoid unhealthy food additives that lead to weight gain or increased inflammation, like high fructose corn syrup and carrageenan.
Consume probiotic-rich fermented foods.
Probiotics are a great way to boost healthy bacteria in the gut, and when it comes to long-term weight loss, your gut is a great place to start. Studies show that an unhealthy microbiome may be a factor in not only the severity of PCOS symptoms, but also the development of the condition.
Add probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi to your diet to do your gut a favor. If you love all things pickled, this is an easy one!
Avoid restrictive diets.
Weight management with PCOS is about playing the long game. Restrictive diets that lead to rapid weight loss in the short term likely won’t work in the long term. Make gradual, sustainable changes to your diet, and embrace more mindful eating.
There’s one exception, though. Variations of intermittent fasting can help with weight loss and PCOS in some women, although it’s not for everyone. It’s also important not to fast for over 14 hours at a time, as this can negatively affect your menstrual cycles.
Talk to your physician about whether you should test it out before you start.
2. Improve your sleep quality.
You need good, quality sleep for long-term PCOS weight loss. That’s typically about 7-9 hours for most adults.
Practice good sleep hygiene to prep your body for a good night’s sleep:
- Keep a consistent sleep schedule (specifically, go to bed at the same time each night)
- Maintain a calm sleep environment
- Avoid staring at screens in the hour before bedtime (that blue light from your phone can affect circadian rhythms and stimulate your brain when it should be shutting down)
- Don’t eat within about 2 hours of your bedtime
- Avoid coffee within 8 hours of bedtime
- Minimize alcohol drinking, and don’t use booze as a way to fall asleep (it causes more restless sleep, even if you fall asleep faster)
If you’re having trouble getting enough rest, talk to your primary care doctor. PCOS and obesity are both risk factors for obstructive sleep apnea.
3. Exercise more effectively.
If you have PCOS, it’s a good idea to get at least 150 minutes of physical activity per week (at least 20 minutes per day).
While it’s common to bust your butt at the gym doing sweaty cardio, that’s not the only (or even the best) type of exercise for you. Focus less on tracking calorie deficits and more on building a strong body.
Resistance training, in particular, is linked to better PCOS outcomes. That doesn’t necessarily mean weight lifting — you can use your body weight to develop stronger muscles.
High-intensity interval training (HIIT) led to better insulin resistance and body composition in a 2015 study of women with PCOS.
Yoga may also help to improve hip and tummy size for PCOS patients, according to a 6-week randomized controlled trial including 61 women.
Just remember: It’s more important to get moving than to feel chained to one specific type of exercise.
If you’re not already physically active, ramp up your habits slowly. Daily walks are great, while daily CrossFit sessions at the gym right away might set you up for failure and potential injury.
4. Practice stress relief and mindfulness techniques.
Chronic stress can impact sleep quality, increase inflammation in the body, and put you at risk for mental health conditions like depression and anxiety. Find ways to reduce overall stress that work for you.
Practicing mindfulness techniques, such as deep breathing and regular meditation, may reduce PCOS symptoms and improve overall wellness.
5. Participate in a group weight loss program for women with PCOS.
Losing weight can be hard to do on your own. Add an endocrine disorder into the mix, and it may very well feel like an unachievable goal.
A group weight loss program for women with PCOS is a research-backed strategy that can help jump-start your weight loss journey.
Our model at SoWell includes both solo and shared medical visits to give you individualized support as you need it with an added layer of support and accountability.
We also use FDA-approved weight loss medications when appropriate to help you reach your milestones. (Scroll down to #10 below to learn more about how they can help.)
Join our group program for 1:1 medical management, group coaching, FDA-approved medications, and unlimited access to our team for long-term weight loss success.
6. Take high-quality supplements that actually work.
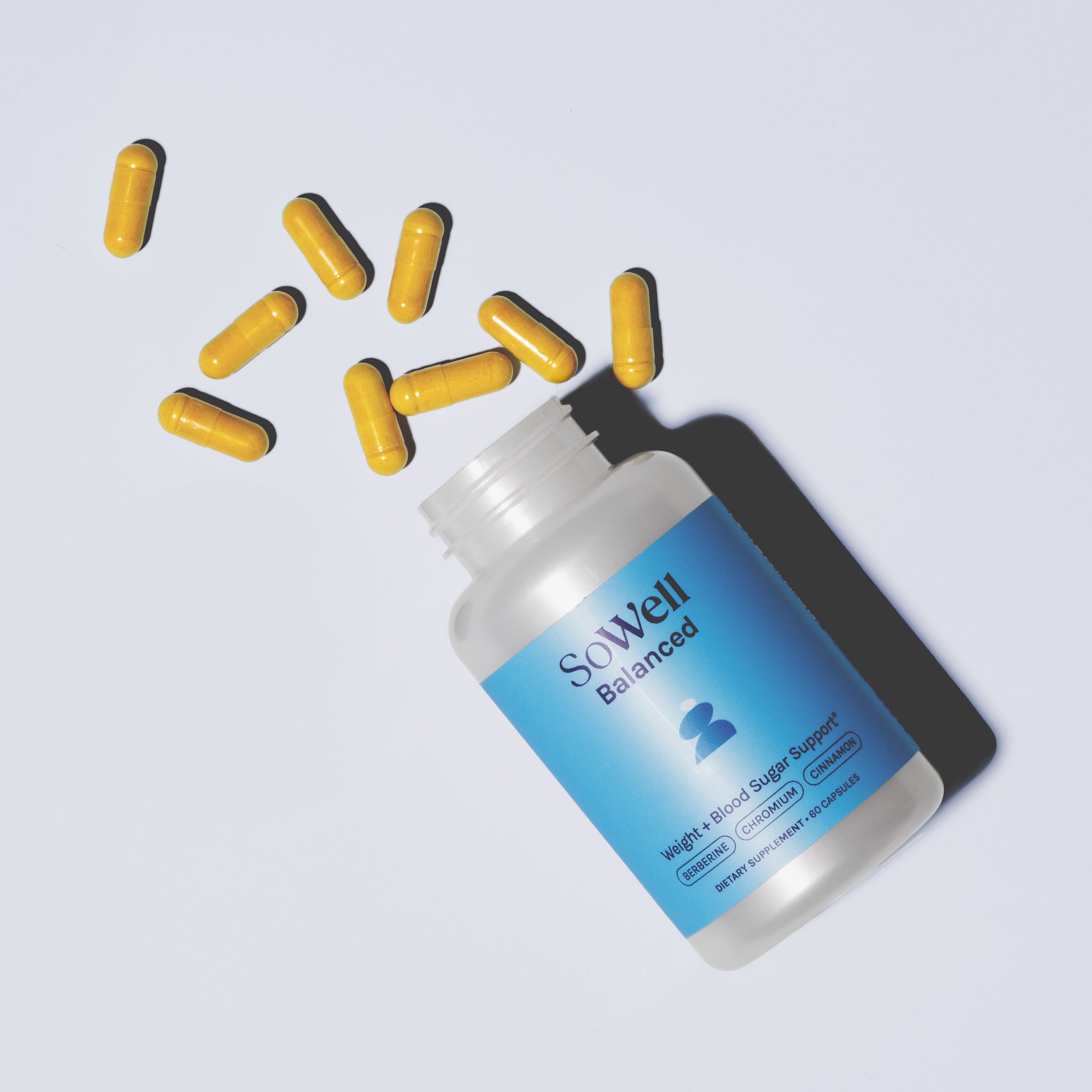
If you’re still struggling to lose weight or keeping your diet in check as you make your lifestyle changes, a supplement can support those efforts.
- Probiotics may have a positive effect on your weight, metabolism, gut health, and several symptoms of PCOS.
- Chromium helps to balance insulin levels, reduce BMI, and decrease testosterone levels in patients with polycystic ovary syndrome. In a study comparing it to metformin, chromium demonstrated similar results with fewer side effects than the prescription drug.
- Berberine also performs comparably to metformin for improving insulin sensitivity and fertility, according to a meta-analysis of 9 clinical trials. Although it may not be directly linked to weight loss, berberine may help to alter body composition and and reduce certain types of fat tissue.
- Cinnamon may reduce insulin resistance and improve cholesterol, blood sugar, and triglyceride levels in patients with PCOS. Some studies suggest it also supports weight loss, but results are inconsistent.
- Folic acid (vitamin B9) may be able to reduce BMI and overall weight for people with PCOS.
- Inositol (myo-inositol and D-chiro-inositol) can support healthy ovarian function and, in some cases, aid PCOS weight loss.
Our GetSoBalanced is formulated to support healthy levels of insulin and cholesterol and overall metabolic health. If you want to target ovarian health, try our GetSoSynced. This natural blend of ingredients supports healthy hormone levels, insulin resistance, and ovarian health.*
Note that dietary supplements aren’t a replacement for a healthy lifestyle. They’re meant to support your journey toward long-term changes for overall wellness.
7. Test your thyroid levels.
Women with PCOS are more likely to show signs of thyroid dysfunction, specifically hypothyroidism. An underactive thyroid can cause weight gain and make it harder to lose weight.
Talk to your doctor about checking thyroid levels to rule it out as a cause of your weight gain. If you have an underactive thyroid, discuss treatment options with your physician.
On the fence about trying a biology kit to expose the underlying cause of your weight gain or difficulties dropping pounds? SoWell’s Weight Biology Kit tests for TSH levels to understand how your thyroid may play a role.
8. Consider therapy to combat emotional barriers.
There may be more standing in the way of long-term weight loss than your lifestyle choices. Consider any emotional barriers at play, then seek out strategies to address what you’re feeling on what can often be a difficult journey.
A combination of nutrition advice, exercise, and cognitive behavior therapy (CBT) can be powerful for women with PCOS struggling to lose weight.
9. Discuss bariatric surgery with your healthcare provider.
If you’ve tried everything else and are still struggling with PCOS and a variety of obesity-related complications, you may want to talk to your doctor about bariatric surgery.
In the most severe cases, surgery can bring fertility back to normal levels more effectively than common PCOS medications like metformin.
Keep in mind that weight-loss surgeries are serious business. You’ll still need to embrace lifestyle changes once you’re out of the operating room to prevent future weight gain and manage PCOS in the long term.
10. Talk to your doctor about medications.
In some cases, doctors may recommend medications to treat PCOS symptoms alongside overall lifestyle changes.
Metformin, a prescription medication used for patients with type 2 diabetes, is often recommended to improve your body’s response to glucose. Some doctors pair it with a low dose of spironolactone, a diuretic that may positively affect testosterone levels and manage male-pattern hair growth.
Hormonal birth control and oral contraceptives may also help some women balance hormone levels in the body, but they may not be recommended if you have a history of blood clots.
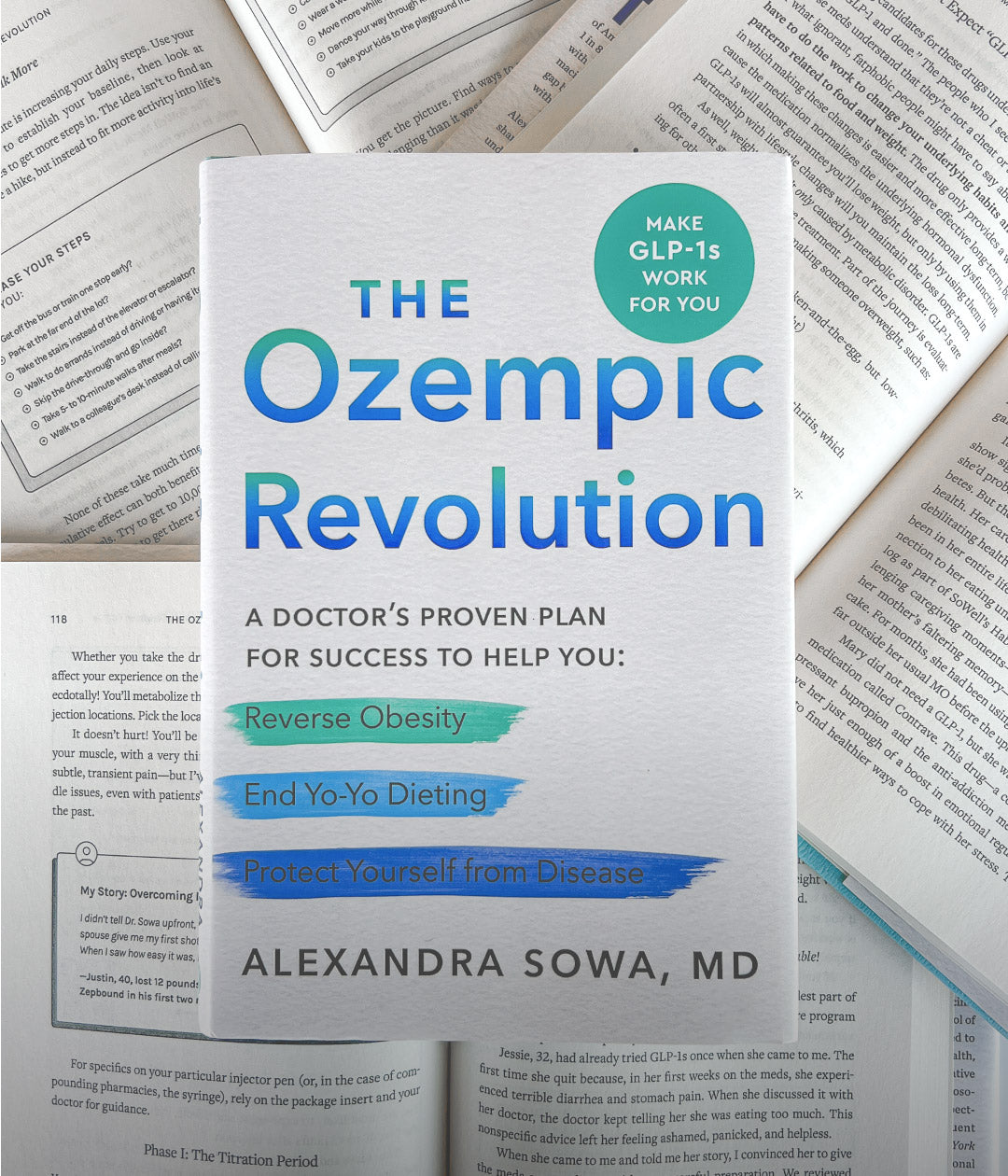
If your weight is the focus, FDA-approved weight loss medications may give you the jump-start you need. The key here is an individualized approach.
Medicine sometimes sounds like a last-resort option, but strategic medication use under the guidance of a physician can empower you to take charge of your weight loss journey. That’s why we use medication in addition to shared medical visits in our group weight loss program.
Yes, you can lose weight with PCOS… and we’re here to help along the way.
You can take control of your PCOS symptoms and lose weight with PCOS, especially when you know help is out there. If you feel like you’re in a hamster wheel and unsure of what to do next, we can help you get well and stay well.
At SoWell, we’ll help you pinpoint the obstacles in your way. It may be that you’re doing all the right things, but metabolic factors are getting in the way. In that case, our Weight Biology Kit can help you figure out your next steps by assessing relevant biomarkers.
Learn more about your metabolic function. Get individualized support with your PCOS symptoms. Feel better long-term.
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Sources
- McGowan, M. P. (2011). Polycystic ovary syndrome: a common endocrine disorder and risk factor for vascular disease. Current Treatment Options in Cardiovascular Medicine, 13(4), 289-301.
- Rojas, J., Chávez, M., Olivar, L., et al. (2014). Polycystic ovary syndrome, insulin resistance, and obesity: navigating the pathophysiologic labyrinth. International Journal of Reproductive Medicine.
- Muharam, R., Purba, J. S., Hestiantoro, A., et al. (2018). Profile on personality types and cortisol in polycystic ovarian syndrome. Middle East Fertility Society Journal, 23(3), 189-194.
- Tasali, E., Van Cauter, E., & Ehrmann, D. A. (2008). Polycystic ovary syndrome and obstructive sleep apnea. Sleep Medicine Clinics, 3(1), 37-46.
- Glueck, C. J. & Goldenberg N. (2018). Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism, 92, 108-120.
- Lim, S., Smith, C. A., Costello, M. F., et al. (2019). Barriers and facilitators to weight management in overweight and obese women living in Australia with PCOS: a qualitative study. BMC Endocrine Disorders, 19(1), 106.
- Mei, S., Ding, J., Wang, K., et al. (2022). Mediterranean diet combined with a low-carbohydrate dietary pattern in the treatment of overweight polycystic ovary syndrome patients. Frontiers in Nutrition, 9.
- Sørensen, L. B., Søe, M., Halkier, K. H., et al. (2012). Effects of increased dietary protein-to-carbohydrate ratios in women with polycystic ovary syndrome. The American Journal of Clinical Nutrition, 95(1), 39-48.
- Paoli, A., Mancin, L., Giacona, M. C., et al. (2020). Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. Journal of Translational Medicine, 18(1), 104.
- Cutler, D. A., Pride, S. M., & Cheung, A. P. (2019). Low intakes of dietary fiber and magnesium are associated with insulin resistance and hyperandrogenism in polycystic ovary syndrome: A cohort study. Food Science & Nutrition, 7(4), 1426-1437.
- Perelman, D., Coghlan, N., Lamendola, C., et al. (2017). Substituting poly- and mono-unsaturated fat for dietary carbohydrate reduces hyperinsulinemia in women with polycystic ovary syndrome. Gynecological Endocrinology, 33(4), 324-327.
- Yurtdaş, G. & Akdevelioğlu Y. (2020). A new approach to polycystic ovary syndrome: The gut microbiota. Journal of the American College of Nutrition, 39(4), 371-382.
- Li, C., Xing, C., Zhang, J., et al. (2021). Eight-hour time-restricted feeding improves endocrine and metabolic profiles in women with anovulatory polycystic ovary syndrome. Journal of Translational Medicine, 19(1):148.
- Arshad, D., Joyia, U. M., Fatima, S., et al. (2021). The adverse impact of excessive smartphone screen-time on sleep quality among young adults: A prospective cohort. Sleep Science, 14(4), 337-341.
- Woodward, A., Klonizakis, M., & Broom, D. (2020). Exercise and polycystic ovary syndrome. Advances in Experimental Medicine & Biology, 1228, 123-136.
- Kogure, G. S., Miranda-Furtado, C. L, Silva, R. C., et al. (2016). Resistance exercise impacts lean muscle mass in women with polycystic ovary syndrome. Medicine & Science in Sports & Medicine, 48(4), 589-598.
- Almenning, I., Rieber-Mohn, A., Lundgren, K. M., Shetelig Løvvik, T., Garnaes, K. K., & Moholdt, T. (2015). Effects of high intensity interval training and strength training on metabolic, cardiovascular and hormonal outcomes in women with polycystic ovary syndrome: a pilot study. Plos one, 10(9), e0138793.
- Mohseni, M., Eghbali, M., Bahrami, H., Dastaran, F., & Amini, L. (2021). Yoga effects on anthropometric indices and polycystic ovary syndrome symptoms in women undergoing infertility treatment: a randomized controlled clinical trial. Evidence-Based Complementary and Alternative Medicine, 2021.
- Kara, O., Kaymaz, N., & Uzun, M. E. (2022). The effect of hyperandrogenism and obesity on mindfulness and metacognition in adolescents with polycystic ovary syndrome. Archives of Women’s Mental Health, 25(5), 911-921.
- Stefanaki, C., Bacopoulou, F., Livadas, S., Kandaraki, A., Karachalios, A., Chrousos, G. P., & Diamanti-Kandarakis, E. (2015). Impact of a mindfulness stress management program on stress, anxiety, depression and quality of life in women with polycystic ovary syndrome: a randomized controlled trial. Stress, 18(1), 57-66.
- Lim, S. S., Hutchison, S. K., Van Ryswyk, E., et al. (2019). Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews, 3(3).
- Tabrizi, R., Ostadmohammadi, V., Akbari, M., et al. (2022). The effects of probiotic supplementation on clinical symptom, weight loss, glycemic control, lipid and hormonal profiles, biomarkers of inflammation, and oxidative stress in women with polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled trials. Probiotics & Antimicrobial Proteins, 14(1), 1-14.
- Fazelian, S., Rouhani, M. H., Bank, S. S., & Amani, R. (2017). Chromium supplementation and polycystic ovary syndrome: A systematic review and meta-analysis. Journal of trace elements in medicine and biology, 42, 92-96.
- Amooee, S., Parsanezhad, M. E., Shirazi, M. R., Alborzi, S., & Samsami, A. (2013). Metformin versus chromium picolinate in clomiphene citrate-resistant patients with PCOs: A double-blind randomized clinical trial. Iranian journal of reproductive medicine, 11(8), 611.
- Li, M. F., Zhou, X. M., & Li, X. L. (2018). The effect of berberine on polycystic ovary syndrome patients with insulin resistance (PCOS-IR): a meta-analysis and systematic review. Evidence-Based Complementary and Alternative Medicine, 2018.
- Rondanelli, M., Infantino, V., Riva, A., Petrangolini, G., Faliva, M. A., Peroni, G., … & Perna, S. (2020). Polycystic ovary syndrome management: a review of the possible amazing role of berberine. Archives of Gynecology and Obstetrics, 301(1), 53-60.
- Maleki, V., Faghfouri, A. H., Tabrizi, F. P. F., Moludi, J., Saleh-Ghadimi, S., Jafari-Vayghan, H., & Qaisar, S. A. (2021). Mechanistic and therapeutic insight into the effects of cinnamon in polycystic ovary syndrome: a systematic review. Journal of ovarian research, 14(1), 1-14.
- Jafari, A., Gholizadeh, E., Sadrmanesh, O., Tajpour, S., Yarizadeh, H., Zamani, B., & Sohrabi, Z. (2022). The effect of folic acid supplementation on body weight and body mass index: a systematic review and meta-analysis of randomized controlled trials. Clinical Nutrition ESPEN.
- Gerli, S., Papaleo, E., Ferrari, A., & Di Renzo, G. C. (2007). Randomized, double blind placebo-controlled trial: effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur Rev Med Pharmacol Sci, 11(5), 347-354.
- Singla, R., Gupta, Y., Khemani, M., et al. (2015). Thyroid disorders and polycystic ovary syndrome: An emerging relationship. Indian Journal of Endocrinology & Metabolism, 19(1), 25-29.
- Jiskoot, G., Timman, R., Beerthuizen, A., et al. (2020). Weight reduction through a cognitive behavioral therapy lifestyle intervention in PCOS: The pimary outcome of a randomized controlled trial. Obesity, 28(11), 2134-2141.
- Hazlehurst, J. M., Singh, P., Bhogal, G., et al. (2022). How to manage weight loss in women with obesity and PCOS seeking fertility? Clinical Endocrinology, 97(2), 208-216.
- Mazza, A., Fruci, B., Guzzi, P., et al. (2014). In PCOS patients the addition of low-dose spironolactone induces a more marked reduction of clinical and biochemical hyperandrogenism than metformin alone. Nutrition, Metabolism, & Cardiovasc Diseases, 24(2), 132-139.
- Oguz, S. H. & Yildiz, B. O. (2021). An update on contraception in polycystic ovary syndrome. Endocrinology & Metabolism, 36(2), 296-311.