When it comes to weight management, we've all heard the same advice: "You just need more willpower." This oversimplified view has dominated weight loss conversations for generations. But what if willpower isn't the answer? Scientific research reveals that obesity is fundamentally a biological condition, one where complex hormonal systems play a far more significant role than mental determination.
Your Body's Hidden Control Room
The human body operates through an intricate network of hormonal signals that regulate hunger, fullness, and metabolism. These chemical messengers work continuously between your brain, gut, and fat tissue to maintain energy balance. But this system's functioning isn't just about what you eat or how much you exercise – it's deeply influenced by your genetic makeup, your family history, and even environmental factors that can modify how your genes express themselves.
Research has uncovered more than 500 genes linked to weight regulation, and studies of twins and adopted children have shown that genetic inheritance accounts for approximately 70% of our body's tendency to gain or maintain weight. The remaining 30% is influenced by environmental factors, which themselves can trigger lasting changes in how our genes function – a phenomenon known as epigenetics.
This complex system can become disrupted for numerous biological reasons: hormonal changes during pregnancy or menopause, certain medications, chronic stress, sleep disorders, autoimmune conditions, or thyroid dysfunction. Even seemingly unrelated factors like your gut microbiome composition or exposure to endocrine-disrupting chemicals in the environment can impact your body's weight regulation system. When these disruptions occur, no amount of mental fortitude can override these powerful biological signals.

The Biology Behind the Struggle
Understanding the complexity of these biological systems reveals why the "just eat less and move more" mantra falls short. For many people struggling with weight, their hormonal system has become fundamentally dysregulated. The body's leptin signaling – which should tell your brain you're full – becomes resistant, much like how some people become resistant to insulin. Meanwhile, ghrelin, your primary hunger hormone, can remain elevated even after eating, driving persistent hunger regardless of willpower.
What Really Happens When You Diet
When someone reduces calories significantly, their body initiates a cascade of biological responses. Hunger hormones surge as a survival mechanism. The metabolism adapts by becoming more efficient – essentially doing more with less energy. Perhaps most challenging, the brain's reward centers become hypersensitive to food cues, making dietary choices increasingly difficult. This isn't a failure of willpower – it's sophisticated biological programming working exactly as designed to prevent what your body perceives as dangerous weight loss.
Modern Medical Understanding
Today's obesity medicine recognizes that while lifestyle changes matter, they often can't overcome these biological adaptations alone. Just as we wouldn't expect someone with diabetes to control their blood sugar through diet alone, we now understand that sustainable weight management typically requires medical intervention to address these underlying hormonal imbalances.
This understanding has led to one of the most significant breakthroughs in obesity medicine: GLP-1 medications. These medications work by targeting the body's complex hormone systems directly. They help regulate hunger signals, improve insulin sensitivity, and assist in resetting the body's weight regulation mechanisms. By mimicking your body's natural hormones, GLP-1s can help restore balance to disrupted metabolic systems.
The success of GLP-1 medications represents a paradigm shift in obesity treatment. Instead of relying solely on willpower to overcome powerful biological signals, we can now provide medical support that works with your body's natural systems. This medical support makes lifestyle changes more achievable and sustainable by aligning your biology with your health goals.
Moving Beyond the Myth
Understanding weight management as primarily biological rather than behavioral transforms how we approach treatment. It shifts the conversation from one of personal failure to one of medical support, from shame to science, and from simplistic solutions to comprehensive care.
This doesn't diminish the importance of healthy lifestyle choices – they remain crucial. But by acknowledging the complex biology at play, we can pursue more effective, science-based solutions that support long-term success. It's time to move past the willpower myth and embrace what science has revealed: successful weight management comes from understanding and working with our biology, not fighting against it.
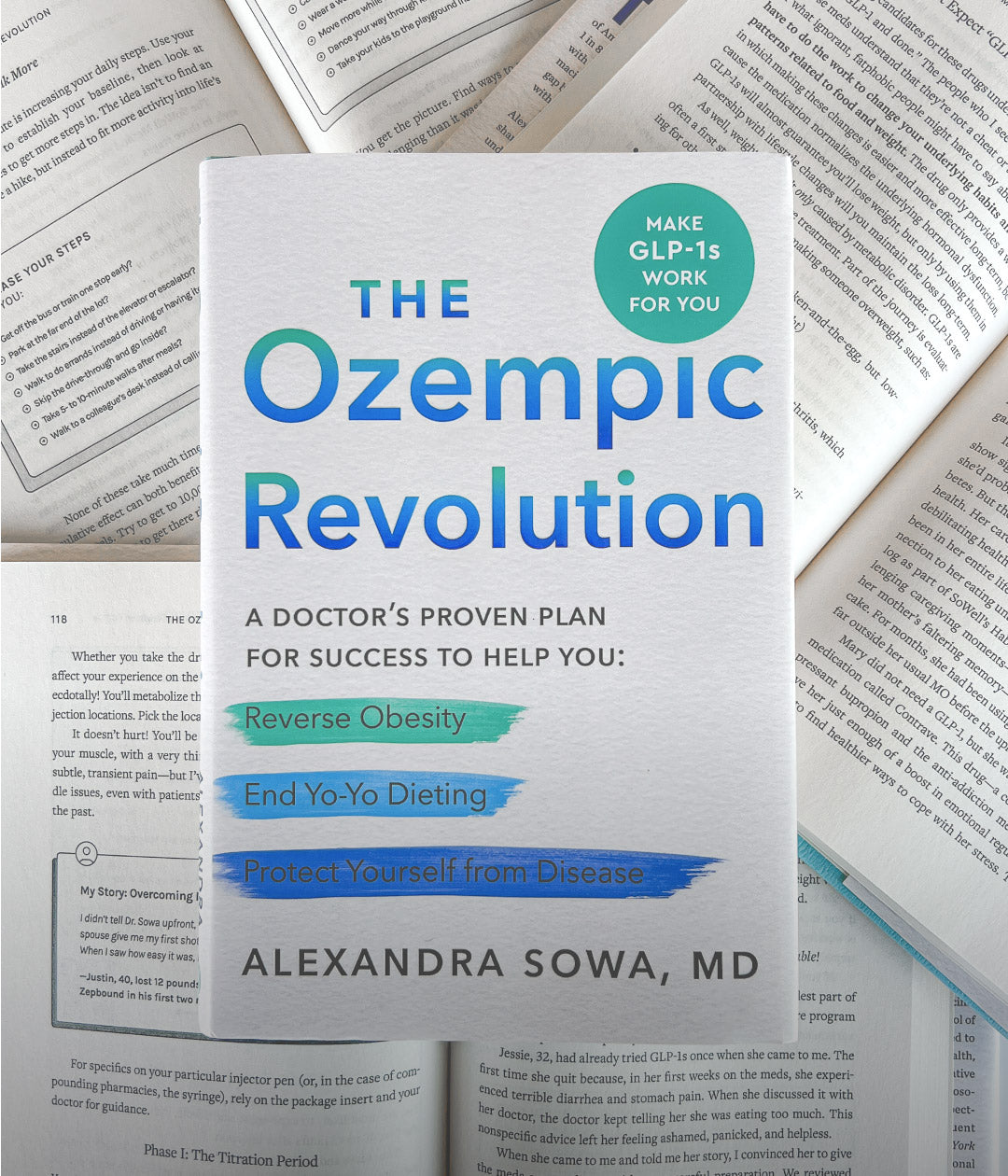
The Ozempic Revolution
Available for pre-order
This groundbreaking book dives into the science and real-world impact of GLP-1 medications, transforming how we think about weight loss and metabolic health. A must-read for anyone in the medical or wellness field.
Shop Now